Benign prostatic hyperplasia (BPH), commonly known as prostate enlargement, is extremely common in men, especially as they age. While most well-known symptoms are urinary—difficulty starting urination or a weak stream—many patients wonder about a more intimate aspect: does an enlarged prostate affect a man sexually?
The short answer is yes, but the issue is complex and deserves careful examination. Although benign, BPH can closely intertwine with sexual quality of life, influencing libido, erection, and ejaculation. Fortunately, with accurate diagnosis and modern therapies, it’s possible to effectively manage both urinary and related sexual issues. In this article, we’ll explore this connection in depth, answer the most common questions, and outline the cutting-edge diagnostic and treatment approaches offered by Prof. Fabio Castiglione at his London clinic.
What is Benign Prostatic Hyperplasia (BPH)?
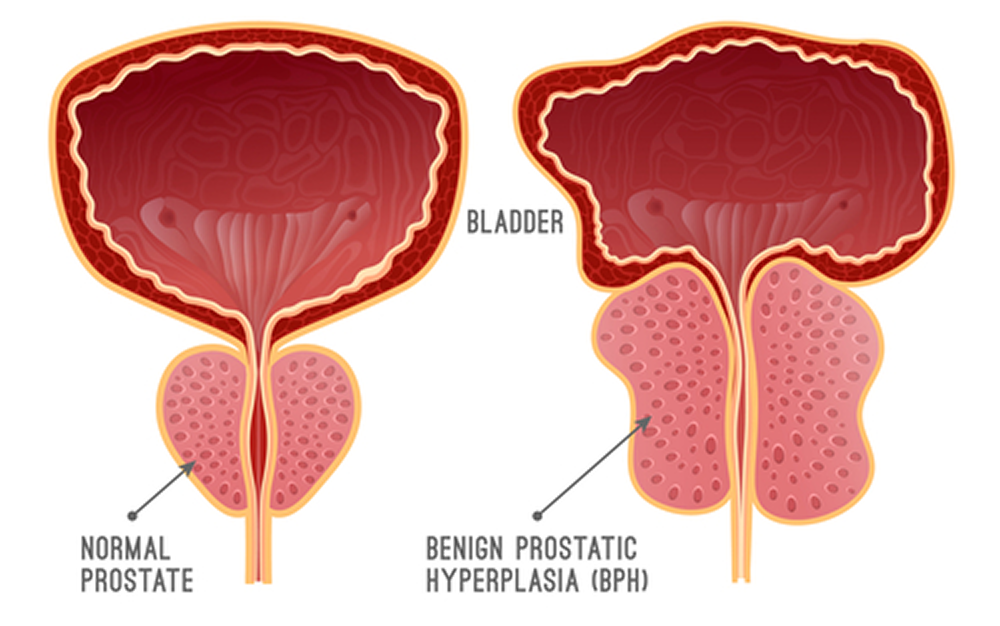
To understand the sexual impact, we must first define BPH. The prostate is a small, walnut-sized gland located just below the bladder and in front of the rectum. Its main function is to produce seminal fluid, which nourishes and transports sperm. The urethra, the channel carrying urine from the bladder out of the body, runs through the center of the prostate. With aging, prostate enlargement is normal. This process—benign prostatic hyperplasia—is not cancer and does not increase prostate cancer risk. However, the growing gland can compress the urethra, causing classic urinary symptoms (LUTS—Lower Urinary Tract Symptoms).
Key risk factors include:
- Age: The single most significant factor. BPH is rare before 40, affects ~50% of men aged 51–60, and up to 90% of those over 80.
- Family history: Having a first-degree relative with BPH increases one’s risk.
- Lifestyle: Obesity, inactivity, and conditions like type 2 diabetes appear to contribute to BPH development and progression.
How does prostate enlargement affect sexual function?

The link between BPH and sexual dysfunction is multifactorial, involving both physiological and psychological elements. Several complex mechanisms, centered on the prostate, explain the impact on male urogenital function.
Physiological and psychological mechanisms
Compression by an enlarged prostate isn’t limited to the urethra. It can affect the nerves and blood vessels crucial for erection. Reduced penile blood flow and altered nerve signaling make achieving or maintaining an erection harder. Additionally, urinary symptoms themselves—such as nocturia (nighttime urination)—cause chronic fatigue and irritability, lowering libido. The psychological impact—health worries, performance anxiety, and self-esteem loss—can create a vicious cycle, worsening sexual difficulties.
Does an enlarged prostate affect a man sexually? Tackle the issue with specialist help from Prof. Fabio Castiglione. Book a consultation: +447830398165.
The most common sexual effects of BPH
Men with BPH may experience:
- Erectile Dysfunction (ED): Difficulty achieving or maintaining an erection is one of the most frequent complaints. Evaluation of BPH should always include assessment of erectile function.
- Reduced Libido: Desire may decline due to hormonal factors, the psychological burden of symptoms, and side effects of some BPH medications.
- Ejaculation Problems: Ejaculation may become painful, or retrograde (semen enters the bladder instead of exiting), or the volume of ejaculate may decrease.
Frequently Asked Questions

At the Erectile Dysfunction Clinic London, Prof. Castiglione hears these questions every day. Here are clear answers:
Can I still have erections with an enlarged prostate?
Absolutely yes. Prostate enlargement does not spell the end of sexual activity. Many men with BPH never experience ED. However, a statistical and physiological correlation exists. The good news: by treating BPH and directly addressing erectile function, you can often significantly improve—or fully restore—erectile capability.
Can I take Viagra if I have BPH?
Generally, yes. PDE5 inhibitors like Sildenafil (Viagra) and Tadalafil (Cialis) are safe and effective for men with BPH and ED. In fact, daily low-dose Tadalafil is approved to treat both BPH symptoms and ED. However, self-medication is dangerous. Only a specialist like Prof. Castiglione can, after thorough evaluation, determine if these drugs suit you, rule out contraindications, and prescribe the correct regimen—sometimes in combination with other BPH therapies.
What’s the fastest way to shrink an enlarged prostate?
Distinguish “symptom relief” from “volume reduction.” Alpha-blockers provide rapid relief of urinary symptoms—days to weeks—but they do not shrink the gland. 5-alpha-reductase inhibitors (finasteride, dutasteride) reduce prostate size but take months to work. Surgical or minimally invasive procedures offer quicker, definitive volume reduction but involve risks and recovery. A specialist consultation is essential to choose the best path.
Which drinks should I avoid with BPH?
Modifying habits can significantly improve symptoms.
Ten drinks to limit or avoid:
- Coffee & caffeinated tea: Caffeine irritates the bladder.
- Alcohol: Increases urine production and worsens symptoms.
- Sugary sodas: Sugar and artificial sweeteners can irritate.
- Citrus juices: Acidity may irritate the urinary tract.
- Energy drinks: High in caffeine and sugar.
- Hot chocolate: Contains caffeine, irritant potential.
- Dairy: May exacerbate inflammation in some men.
- Tonic water: Contains quinine, which can provoke bladder spasms.
- Ice-cold beverages: May trigger bladder spasms in sensitive individuals.
- Large fluid intake before bedtime: To reduce nocturia, spread fluids through the day.
Does an enlarged prostate affect a man sexually? Find out with Prof. Fabio Castiglione. Call London: +447830398165.
BPH vs. Prostatitis: Not the Same
It’s easy to confuse BPH with prostatitis, but they differ and affect sexuality differently.
- BPH: Age-related, non-inflammatory enlargement. Symptoms are mainly urinary (weak stream, frequency). Sexual impact is often vascular/neural.
- Prostatitis: Inflammation or infection, any age. Symptoms include pelvic pain, painful urination, sometimes fever. Sexually, pain during or after ejaculation can lead to sexual avoidance.
Accurate differential diagnosis by a urologist-andrologist is crucial.
Diagnostic Pathway: Prof. Castiglione’s Method

Addressing sexual issues linked to BPH requires more than prescribing medication. Prof. Fabio Castiglione uses a comprehensive diagnostic protocol:
- Detailed history: Thorough urological and sexual health interview.
- Validated questionnaires (IPSS, IIEF-5): Objectively measure urinary and erectile function.
- Physical exam: Including digital rectal exam for prostate size/consistency.
- Blood tests (PSA): To rule out other conditions and monitor prostate health.
- Uroflowmetry: Measures urine flow strength and volume.
- Transrectal prostate ultrasound: Precisely images prostate size and internal structure.
This integrated approach yields a precise diagnosis!
Personalized Treatment Approaches
Once diagnosed, Prof. Castiglione tailors therapy from:
Pharmacological Options
- Alpha-blockers for urinary relief
- 5-alpha-reductase inhibitors to reduce prostate volume
- PDE5 inhibitors (e.g. daily Cialis) for both BPH and ED
Regenerative & Non-Invasive Therapies
- Low-intensity shockwaves applied to prostate and penis to reduce inflammation, improve blood flow, and stimulate tissue regeneration.
- P-Shocks (PRP + Shockwaves): Prof. Castiglione’s signature protocol. Combines shockwaves with autologous PRP injections—rich in growth factors—to repair tissue and promote angiogenesis, tackling both urinary and sexual dysfunction at their vascular roots.
- Lifestyle advice: Anti-inflammatory diet, pelvic floor exercises, weight management to optimize results.
Regain Sexual Well-Being
In conclusion, prostate enlargement can impact men’s sexual health, but it need not be a life sentence. The link between BPH, ED, low libido, and ejaculatory issues is well documented. Yet modern medicine offers a broad arsenal—from tailored medications to innovative regenerative therapies (shockwaves, P-Shocks). Confronting the issue with an experienced urologist-andrologist is the first, vital step to restore both urinary health and a fulfilling sex life. Don’t let BPH compromise your intimacy. Contact Prof. Fabio Castiglione in London today: +447830398165 or book online.