Male Fertility Clinic
Holistic Andrology male fertility clinic is here to support men in their greatest desire: having a child. We offer would-be parents a structured programme created around their needs, ensuring highly specialized staff, innovative technologies and comfortable environments.
Holistic Andrology provides a safe place and a transparent, supportive relationship even when the treatment is challenging.
Dr Castiglione manages patients with male infertility. He carefully selects patients in whom surgical or medical therapies can result in a stable seminal improvement and who, therefore, have a good chance of spontaneous conception in a reasonably short time.
An essential component in this work is also to provide couples with precise and truthful information regarding the realistic expectations of the success of the proposed treatments. In general, the andrologist's approaches aim to improve the seminal parameters (number, motility and morphology of the spermatozoa). Their expert evaluation can approximate the probability of a spontaneous pregnancy in the couple in question.
Indeed, assessment of a couple with infertility must also consider the characteristics of the female partner — for example, the age of the woman, previous fertility, tubal patency or endometriosis — which can strongly influence the success rates of any male treatment.
When conditions associated with a reasonable probability of spontaneous fertilisation have been excluded, treatment progression to low-technology (intrauterine homologous insemination = IUI) or high-technology (IVF or ICSI) assisted fertilisation techniques might be necessary. If sperm quality cannot be sufficiently improved with either medical or surgical therapies, assisted fertilisation (ICSI, for the most part) remains the only possible treatment.
In men with azoospermia (the absence of spermatozoa in the seminal fluid) or in men who are unable to ejaculate for psychological or neurological reasons, surgical, microsurgical or minimally invasive instrumental techniques can often be successful in recovery of sperm from the seminal tracts for use in ICSI.

Four groups of treatable diseases can be responsible for male infertility..
Varicocele can be responsible for secretory changes in the gonad. This pathology is present in 35% of males with primary infertility and 81% of cases of secondary infertility. Correction of varicocele improves semen quality in 60–80% of patients and can result in spontaneous conception rates of 43% within the first year and 69% within the second year after surgery.
The second group includes obstructions of the proximal seminal passages, which include the rete testis, efferent cones, epididymal tubules and vas deferens. These pathologies are often a consequence of sub-acute epididymitis (for example caused by chlamydia): an inflammatory process is established, which causes scar formation that strangles the epididymal tubules resulting in obstruction. The upstream tubules gradually dilate until they rupture, causing extravasation of spermatic material into the interstitium, which, in turn, triggers a further inflammatory reaction in a cascade effect. Medical therapies are usually ineffective for the treatment of this disorder.
In the presence of complete bilateral obstruction of the epididymis, azoospermia occurs In the presence of azoospermia, most centres offer systematic ICSI using spermatozoa obtained from testicular aspiration. However, in carefully selected patients, we offer the couple the much more physiological option of tubule microsurgical vasostomy. According to the biggest series published so far, microsurgical tubule vasostomy leads to recanalisations in 70% and spontaneous conception in 36% (at various follow-up points).
In the presence of obstruction of the proximal vas deferens, which is often seen in men who have previously had a vasectomy, microsurgical vaso-vasostomy is used, which results in recanalisation in 80–93% of cases and spontaneous pregnancy in 52–82% of couples. The rates are slightly lower (50–65% and 43%, respectively) in cases of vas deferens obstruction arising after previous surgical interventions such as hernioplasty.
This group also includes obstructions of the distal seminal passages (seminal vesicles, deferential ampullae, and ejaculatory ducts). Acquired anatomical obstructions (or subobstructions) of the distal seminal tracts are often localised to the ejaculatory ducts and can be outcomes of tuberculous or non-specific infectious processes. Other frequent causes are lithiasis (seminal stones wedged in the ducts) and iatrogenic (caused by medical intervention), for example damage to the urethral outlet from previous urethral catheterisation or other endoscopic urological manoeuvres).
Functional obstructions of the distal seminal passages are distinguished by the absence of anatomical alterations of the ejaculatory ducts and are most likely dysfunctions of local neurological origin or systemic. In the presence of anatomical obstruction of the ejaculatory ducts, resection or incision of the ducts is performed via transurethral endoscopy (TURED). The recanalisation rate of this procedure extrapolated from selected international cases is 36%, with a cumulative pregnancy rate of 26%.
In cases where the unblocking of the distal seminal tracts might present even moderate risks for the subsequent health of the patient, surgical recovery of spermatozoa from the testicle is preferred using testicular sperm extraction (TESE), which is associated with very few complications, or testicular fine needle aspiration (TeFNA), which can then be used fresh or cryopreserved for ICSI.
Seminal tract washout (STW) has proven effective in temporarily unblocking the ejaculatory ducts that were affected by seminal stones or thickened material. When obstruction of the ejaculatory ducts is caused by extrinsic compression by Müllerian cysts, we can also perform aspiration–sclerotization of the cyst transrectally under ultrasound guidance (TRUCA).
The third group includes the incorrect positioning of the gonads, caused by hypermobility of the funiculus resulting in thermal or ischaemic damage and, therefore, secretory dysfunction, and of the epididymis, whereby vertical inversion of the epididymis and epididymal–testicular disjunctions, which can be responsible for impaired sperm maturation or functional obstruction of the epididymal tubule. Treatment of these malpositions is ideally performed at a young age or when the malposition causes problems for the patient.
The fourth group includes ejaculatory disorders including, for example, anejaculation or retrograde ejaculation. Ejaculatory disorder can be secondary to a wide range of systemic neuropathies, such as diabetes and multiple sclerosis, or local neuropathies, which include outcomes of post-traumatic paraplegia and tetraplegia, retroperitoneal lymphadenectomy, aorto-iliac surgery, and rectal surgery, which can alter the mechanisms of seminal delivery and ejaculation. In cases of neurogenic retrograde ejaculation, the ejaculation process can sometimes be corrected (anteriorisation) through pharmacological treatments.
Retrograde ejaculation
In case of retrograde ejaculation (It occurs when semen enters the bladder instead of emerging through the penis during orgasm), spermatozoa can be recovered from the bladder using methods tested for two decades, and prepared in a medium suitable for their survival before being used for artificial insemination. In cases of neurological or psychogenic anejaculation, vibration stimulation of the penis or electroejaculation is usually used to collect sperm for artificial insemination.
Vibration massage is an easy, repeatable technique that can be performed in an outpatient clinic or, in selected circumstances, at home. It triggers an anterograde, retrograde or mixed reflex ejaculation through an intense vibratory stimulus focused on the penis. In men with spinal lesions, vibration massage enable collection of spermatic material in 50–60% of patients, which can be used for self-insemination (Cumulative Pregnancy Rate ~ 30%) or low or high technology assisted fertilisation (Cumulative Pregnancy Rate ~ 50%).
For cases of anejaculation that do not respond to these two techniques, TESE or the simpler TeFNA procedures can be performed, in order to collect sperm for assisted fertilisation techniques.
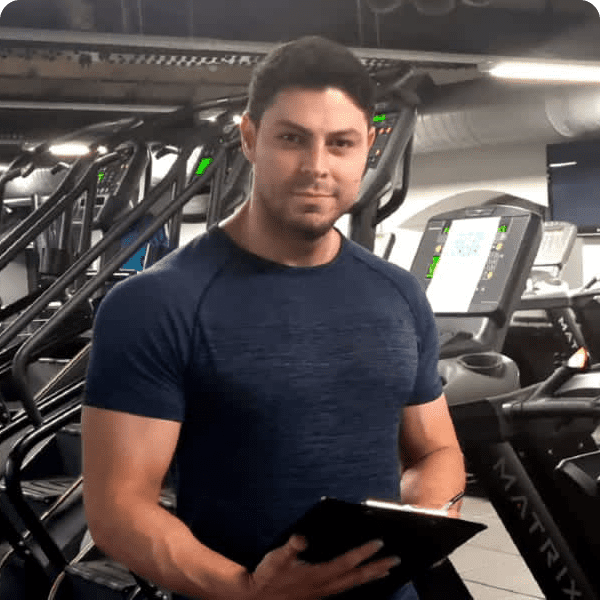
The London Male Fertility Clinic
Modern andrology aims to treat male infertility according to ethical, methodological, organisational and scientific principles. A correct and timely andrological diagnosis is imperative and, where possible, a we create a therapeutic programme for the infertile man to result in spontaneous pregnancies where possible or to move onto inexpensive assisted fertilisation techniques if required.
At Holistic Andrology, we believe that it is not medically or ethically acceptable for couples to be immediately referred for ICSI. This inappropriate early referral for ICSI often happens in clinical practice, and can lead to expensive and physically demanding procedures that might be unnecessary, which is especially important bearing in mind the high economic costs of the procedures and the far from guaranteed positive result of the ICSI itself. Notably, sperm DNA anomalies that are not detectable in the traditionally performed standard seminal examination are often the cause of repeated failures of in vitro fertilisation procedures and, therefore, these should be ruled out or addressed with other therapeutic options before ICSI is considered.