Prostatitis
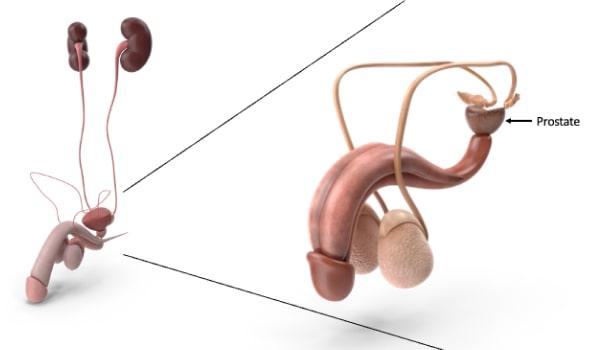
Prostatitis is an inflammation of the prostate gland. The prostate is part of the male genital apparatus and is located just below the bladder. It is similar in shape and size to chestnut and tends to swell with advancing age. The primary prostate function produces and stores seminal fluid released during ejaculation.
Prostatitis should not be confused with prostate cancer since it does not depend on tumour processes or benign prostatic hypertrophy, an abnormal gland enlargement.
Prostatitis can affect any male person. Prostatitis affects 50% of men at some point in their lives, with those aged 30 to 50 most vulnerable. Prostatitis can be:
- Acute, caused by a bacterial infection
- Chronic, caused by a bacterial infection
- Chronic of non-bacterial origin (or chronic pelvic pain syndrome)
- Asymptomatic
Symptoms
The disorders (symptoms) caused by prostatitis vary depending on the type of inflammation. Still, they usually irritate the urinary tract, cause pain in the lower abdomen, sexual problems, and a possible drop in fertility.
Acute prostatitis of bacterial origin generally manifests itself abruptly and suddenly with the typical signs of genitourinary infection, such as:
- Chills
- fever
- Back pain in the genital area and lower back
- The difficulty, irregularities, and pain in the emission of urine (dysuria).
- A recurring urge to urinate, usually at night (nocturia).
- Some people experience pain or burning while urinating.
- Muscle and joint pain, flu-like symptoms
- presence of bacteria in the urine
- presence of blood in the urine (hematuria).
- Chronic prostatitis of bacterial origin is characterised by symptoms that appear gradually. In general, the symptoms are less severe and come and go. There are times when they are especially noticeable and times when they are not.
Chronic prostatitis of non-bacterial origin (or chronic pelvic pain syndrome) manifests symptoms similar to those reported for prostatitis of bacterial origin. The specific features of this form of prostatitis are the absence of bacteria in the urine, sperm, urethral swab and fever. But nothing, in particular, can be found to explain why they show up, and sometimes they go away for a while and then come back without warning.
Asymptomatic prostatitis does not cause pain or discomfort despite signs of inflammation, such as, for example, the presence of white blood cells in the sperm or prostate fluid.
Causes
Therefore, most acute prostatitis of bacterial origin comes from the intestine, particularly Escherichia coli, which is responsible for 50–90% of cases, and from bacteria of the genus Proteus, Klebsiella, Serratia, and Pseudomonas. Other bacteria belonging to the Enterococcus and Staphylococcus species, as well as sexually transmitted microorganisms such as, for example, Neisseria gonorrhoeae, Chlamydia trachomatis, and Ureaplasma urealyticum, are more rarely the cause of prostatitis.
In people who weaken the body's defence system (immunosuppressed or immunodeficient), prostatitis can also be caused by other species of bacteria such as Salmonella, Staphylococcus, and Mycobacterium. If favoured by poor hygiene, weak immune defences, and behavioural factors (such as stress, smoking, alcohol, dietary imbalances, and a sedentary lifestyle), these bacteria can go up the urethra and reach the prostate.

Chronic prostatitis of bacterial origin is, generally, the consequence of a recurrence—that is, of an infection of the prostate that, despite therapy, recurs over time. It is caused by bacteria located in particular areas of the prostate where they are difficult to reach by antibiotics. A factor favouring the eroticization of bacterial prostatitis is the presence of recurrent urinary tract infections.
Chronic prostatitis of non-bacterial origin is the most common form of prostatitis. It can appear at any age but generally affects men over 25. In this type of prostatitis, there are no signs of infection, and despite numerous studies, the factors that determine its onset are not yet fully known. Several hypotheses have been put forward about this disease's origin, including nerve injuries of the lower urinary tract caused by surgery or a traumatic event (for example, a cycling or riding injury), excess stress or psycho-physical overload, heavy work activities, and high-impact sports practice.
Asymptomatic prostatitis is a specific inflammatory disease of the prostate characterised by white blood cells in the spermatic and prostate fluid, a hallmark of an ongoing inflammatory process. This disease is asymptomatic, which means it doesn't cause any symptoms, and no one knows what it is yet.
The assessment (diagnosis) of prostatitis is mainly based on the disorders (symptoms) reported by the patient and on a general physical examination. Once the suspicion of prostatitis is confirmed, it is necessary to undergo laboratory tests on urine and prostate or seminal fluid to identify the possible presence of bacteria. Such examinations, as a rule, are sufficient but, especially in cases of prostatitis of non-bacterial origin, they can be supplemented with a urodynamic test (uroflowmetry), which studies and evaluates the functionality of the bladder and urethra during their tasks of storage (bladder) and release (urethra) of urine, and with transrectal prostate ultrasound, which verifies the size and morphology of the prostate. For prostatitis not caused by bacteria, such as chronic pelvic pain syndrome and asymptomatic prostatitis, white blood cells, even in large numbers, can be found in sperm and urine.
Therapy

Prostatitis therapy depends on its causes, but its elimination is not always straightforward and can take a long time. In the case of acute prostatitis of bacterial origin, the commonly used therapy is antibiotics. The doctor chooses the type of antibiotic, the dose, and the method of administration (posology) most suitable based on the disease severity, the patient's state of health, and his response to therapy. Since the prostate is poorly sensitive to the action of antibiotics, the disease often requires prolonged drug treatment, even for many weeks, using antibiotics or antibacterials capable of penetrating deep into the prostate tissue.
Antibiotic treatment can be accompanied by other drugs to relieve pain (painkillers, such as paracetamol, or non-steroidal anti-inflammatories called NSAIDs, such as ibuprofen) or mitigate urinary disorders by relaxing the smooth muscles of the bladder and prostate (alpha-blockers and supplements).
Treating chronic prostatitis of bacterial origin is based on antibiotic therapy for acute forms. Still, it is more complex because of the poor sensitivity to treatment and the tendency of the infection to recur (relapse). To reduce these risks as much as possible, it is essential to follow the doctor's instructions on how long to take antibiotics and how to take them.
Although there is no specific treatment for prostatitis of non-bacterial origin, people who suffer from it can relieve symptoms using alpha-blocker drugs, painkillers and anti-inflammatories. The use of antibiotics to treat prostatitis of non-bacterial origin (chronic inflammatory pelvic pain syndrome) is a matter of discussion since antibiotic therapy would still seem to have given positive results, even in the absence of detectable bacterial infections.
Asymptomatic prostatitis generally does not require any treatment.
Healing from acute bacterial prostatitis depends on the speed of its discovery and the initiation of appropriate therapy, which almost always resolves the inflammatory state. In contrast, late diagnosis and neglect of medicine can result in chronic inflammation and other complications.
In addition to drugs, simple remedies can help ease the symptoms of prostatitis, such as:
- Baths or wraps that are hot
- Reduction of foods and drinks that can irritate the bladder (alcohol, caffeine, spices, and acidic foods).
- Caffeine-free beverages, especially water, can promote urination and bacteria elimination.
- Avoid sitting for a long time or playing sports that can irritate the prostate, such as cycling.
Maintaining a correct lifestyle is a valuable aid in the prevention of prostatitis. Especially:
- Follow a diet low in fat, salt, and spices and prefer consuming fruits and vegetables.
- Drink plenty of water during the day.
- Avoid or reduce your intake of foods that irritate the bladder, such as alcohol, caffeine, spices, and acidic foods.
- Regular practice of moderate physical activity.
- Keep your body weight under control.
- Take care of intimate hygiene.
- Quickly cures urinary infections.
- Carry out at least one urological examination in each of the following three stages of life: puberty, adulthood, and old age.
In the absence of adequate care or delays in the administration of therapy, acute prostatitis of bacterial origin can become chronic or even be transmitted to nearby organs or tissues (for example, testicles and epididymis). More rarely, the infection can also spread to the blood (bacteremia) and, in severe cases, to the whole organism (sepsis or septicemia). Other problems that can happen with prostatitis are not being able to urinate and getting a prostate abscess, which is a pus-filled hole in the prostate.
Chronic prostatitis that isn't caused by bacteria can cause depression and anxiety, just like many other long-term conditions that cause constant pain, are hard to treat, and tend to come back