Definition and epidemiology
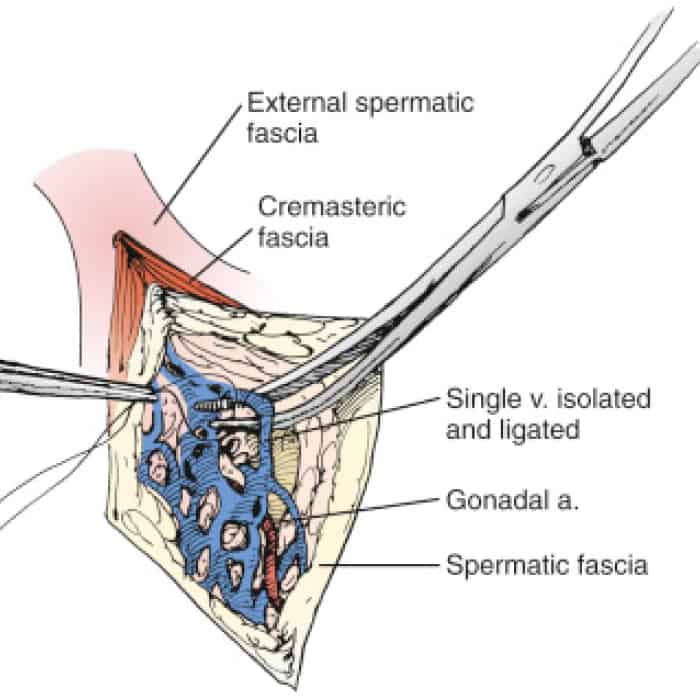
Varicocele surgical ligation
Varicocele is when the veins in the pampiniform plexus get bigger and twisty because of backward flow in the internal spermatic vein.
The idiopathic varicocele is mainly present on the left due to the conformation of the spermatic vein on that side, which enters the renal vein at right angles. Varicocele rarely develops secondary to compression of the renal vein, thrombosis of the renal vein or vena cava, and aneurysm of the abdominal aorta. In all these cases, we speak of secondary varicocele.
About 15% of the general population and 25.4% of partners of subfertile couples (pregnancy did not start after at least one year of unprotected intercourse, in the absence of apparent female causes of reduced fertility) associated with despair (alteration of sperm parameters). The pathophysiological relationship between left varicocele and subfertility, or the mechanism that possibly generates an improvement in fertility after correction of the left varicocele, is still largely undefined. Reduced venous outflow from the testis has been suggested as a possible cause. This can lead to increased scrotal temperature, low oxygen levels, high intra-testicular pressure, and the backflow of adrenal metabolites from the renal vein, which are bad for spermatogenesis.
Clinical diagnosis
It is based on physical examination with the patient in an upright position. Different degrees are distinguished in the detection conditions of varicosity above the testicle:
- Inspection survey, grade III.
- palpation in states of rest; grade II.
- Grade I: palpation only during the execution of the Valsalva manoeuvre.

Obesity, previous surgery, testicular retention, and cremasteric reflex are risk factors. The rationale for this position is that there is a solid relationship with subfertility only for clinical varicocele, therefore diagnosed by physical examination. Even though the physical examination is burdened by subjectivity and extreme inter- or intra-individual variability , international scientific societies' guidelines do not allow for instrumental diagnosis in the subject with couple subfertility and suspected varicocele except in the case of a physical examination
Today's reference instrumental investigation is scrotal doppler ultrasound. Although it provides a more objective and reproducible assessment of the varicocele than physical examination, it is still hampered by the lack of agreement on the method of execution. The diameter of the supra-testicular veins> 3 mm on ultrasound examination using grayscale and the presence of continuous venous reflux at rest on Doppler examination, with or without an increase in Valsalva, are indicative of varicocele.
Healthy subjects without clinical and normozoospermic varicocele demonstrate the constant absence of continuous reflux at rest. At the same time, they have supra-testicular vein diameters comparable to the values indicated in subjects with clinical varicocele. Therefore, the flowmeter parameter seems to be the most discriminating in the instrumental diagnostics of varicocele.
The venography of the internal spermatic vein is highly accurate as a diagnostic test, but it is invasive and exposes the patient to X-rays. Therefore, its use is substantially restricted to cases of varicocele persistence after correction to define the anatomy of reflux in the vessels—spermatic before any new modification.
In conclusion, the diagnosis of varicocele is essentially clinical and based on physical examination. The scrotal echo-color-Doppler examination should be reserved for cases of doubtful classification.
The cause-and-effect relationship between varicocele correction and fertility improvement has been the subject of lively debate. A Cochrane review has shown that in male partners of subfertile couples lacking an apparent female factor, varicocele treatment is associated with an increase in the pregnancy rate compared with non-treatment, particularly evident in the case of disparate subjects and carriers of clinical varicocele. (not in the subclinical one, highlighted only with instrumental examination). The results are not considered conclusive due to the poor quality of evidence defined.
A meta-analysis in endospermic subjects and clinical varicocele, but not in the subclinical, demonstrates a positive effect of varicocelectomy on the concentration and motility of ejaculated spermatozoa.
A negative association between the clinical grade of varicocele and sperm parameters and, after correction, a positive association between the clinical rate of varicocele and improvement of seminal parameters are reported. However, the quality of evidence is modest. Reports show that it increases the number of pregnancies, but only in people who have been infertile for more than two years.
In conclusion, varicocele correction is indicated in partners of subfertile and dyspermic couples, carriers of clinical varicocele, to improve seminal parameters and increase the probability of pregnancy. The usefulness of correcting subclinical varicocele remains questionable.
The correction of varicocele has also been proposed in the treatment of the subject affected by non-obstructive azoospermia (NOA) to improve spermatogenesis and obtain ejaculated spermatozoa to be used by intra-cytoplasmic oocyte injection (ICSI) (12) or to increase the probability of recovery of testicular spermatozoa after a testicular biopsy extraction (TESE) procedure in the case of persistent azoospermia.
Based on 14 retrospective studies, ejaculated spermatozoa were described in 36% of 327 treated subjects.
Overall, with the limited quality of the studies, about 1/3 of patients could avoid recourse to TESE to perform ICSI. A recent prospective study suggests that the pre-varicocelectomy blood level of FSH 10 mIU/mL in azoospermic subjects identified 82.0% of cases with ejaculated spermatozoa, with a specificity of 81.8% and sensitivity of 83.3%. The available data, while promising, does not allow us to provide clinical behaviour indicators.
In conclusion, the correction of clinical varicocele in subjects suffering from NOA can be associated with the appearance of ejaculated spermatozoa, thus avoiding a TESE to carry out ICSI, but it is necessary to define the type of subject in which the probability of success is better, considering that in the presence of azoospermia, delayed use of TESE can harm the success of ICSI if the female partner is> 37 years old.

Spermatic cord
Some observational studies suggest varicocele may be associated with progressive deterioration of seminal parameters and Leydigian function. Although not sufficiently supported, the association of a clinical varicocele with low levels of testosterone mix and reduced volume of the ipsilateral testis is considered an indication for correction.
The documentation of an increase in testosterone mix after varicocelectomy in hypogonadal subjects and partners of subfertile couples supports some indefinite treatment usefulness.
In conclusion, to increase the testosterone mix, varicocelectomy in hypogonadal subjects and subfertile partners is a possible and promising option to be supported with appropriate studies.
The prevalence of varicocele in adolescents is estimated at between 11% and 15%, and in most cases, it is an asymptomatic condition. The relevance of treatment for this condition is controversial. The correction of a clinical varicocele (stage II and stage III) in young people between the ages of 12 and 17 does not seem to have influenced the subsequent probability of paternity compared to the population of untreated boys, even in the case of associated relative hypotrophy. Of the left testicle.
A meta-analysis of 14 studies, mostly retrospective and of poor quality, shows that in 1475 adolescents, the correction of varicocele associated with hypotrophy of the left testis, as the only sign of testicular distress, is associated with a reduction in the level of hypotrophy. For ethical reasons, the lack of adequate reference parameters and the progressive physiological increase in spermatogenesis between 12 and 18 years make the evaluation of seminal parameters impossible in this population of subjects. Based on the changes after treatment, the results of a meta-analysis that says seminal parameters have improved in teenagers after varicocelectomy aren't as clear-cut as they could be.
In conclusion, the correction of varicocele in adolescents should be considered in testicular asymmetry with hypotrophy of the left testicle. Teenagers with a clinical varicocele and normal testicular symmetry should have their testicles measured annually and get a spermiogram at the end of puberty to find early signs of testicular distress.

Varicocele embolization
They include both surgery and interventional radiology.
Lymphatic-sparing micro-surgery is the surgical technique with the lowest complication rate, the lowest failure rate, and the highest pregnancy rate. However, the high cost and the considerable experience required must be considered.
The radiological techniques of retrograde or antegrade phlebography use stents and sclerosing substances positioned in the decidedly varicose veins of the spermatic cord. These procedures are provided outpatient, with a valuable recovery time compared to other methods (just 24 hours). The phlebographic phase of the technique also provides a precise diagnostic evaluation of the dilated vessels and therefore allows a targeted correction of the same. The method does not require general or spinal anaesthesia.
The percentage of testicular atrophy or interstitial oedema is zero since there is no involvement of the arteries or lymphatic vessels. The downside is being exposed to X-rays, the amount of which depends on how experienced the operator is.
Although microsurgical correction of varicocele appears to be the preferred modality, radiological techniques are a valid alternative.
Correction of varicocele: is age relevant?
The effect of age on the results of varicocelectomy is controversial and based solely on retrospective observations. Age plays a negative or neutral role in sperm quality in subfertile subjects treated for clinical varicocele. The role of age in reducing left testicular hypotrophy after varicocelectomy in paediatric age is entirely undetermined. Pending prospective studies, it is advisable to suggest that the correction of clinical varicocele be delayed.
- In adults, in the case of alteration of sperm parameters, regardless of the current search for paternity;
- In paediatric age, in the case of hypotrophy of the left testicle