Sexually transmitted diseases
Sexually transmitted diseases (STDs) or sexually transmitted infections (STIs) are sent by direct contagion through sexual contact. They are typically caused by bacteria, viruses, and protozoa that pass from one individual to another by passing infected biological fluids through the mucous membranes. These pathologies can affect the genital organs or other organs and systems.
What are sexually transmitted diseases?
Sexual activity plays a fundamental role in the spread of these infections. Still, it is possible to become infected even without sexual contact. This is what happens, for example, in the case of transmission from mother to child during pregnancy or childbirth (vertical transmission), through transfusions of infected blood, or through the use of needles or surgical instruments that are not correctly sterilised (tattoos).
Sexually transmitted infections can be caused by:
- Bacteria (gonorrhoea, syphilis, Chlamydia);
- HIV, as well as hepatitis A, B, and C);
- Protozoa (such as trichomoniasis).
- Candida albicans mushrooms
What are the symptoms of sexually transmitted diseases?
Sexually transmitted infections can go unnoticed for a long time. Depending on the type of infection, signs and symptoms may appear anywhere from a few days to a few years after exposure. Some conditions are trivial and resolved in a few days (this is the case, for example, of Candida albicans) or a few weeks without leaving consequences.
Other times (as in the case of HIV or syphilis), the progression of the pathology can lead to severe and sometimes lethal complications. Some of these infections can start without any symptoms and go on for a long time, but they can cause extreme changes in how some organs work, causing them to lose their function. For example, Chlamydia Trachomatis can damage the tubes, leading to infertility.
Particular attention should be paid to certain signs
- Sores on the genitals, in the rectal area or the oral area.
- Some people experience burning or pain when urinating.
- Secretions from the Penis.
- Vaginal discharge (leucorrhea)
- Vaginal blood discharge.
- enlargements the lymph nodes, especially in the groyne area.
- Persistent fevers or diarrhoea, in some cases, may accompany pelvic pain.
- Skin rash on the trunk, hands or feet.

Prevention is essential to avoid the onset of sexually transmitted infections. There are several ways to prevent or reduce the risk of developing these diseases:
- Abstention from sexual activity "at-risk" (avoid casual sexual intercourse, use a condom correctly).
- Vaccinations: It is possible to get vaccinated to prevent infection with Human Papillomavirus (Hpv), hepatitis A, and hepatitis B.
- Avoid the use of drugs or alcohol abuse, the effect of which can favor the adoption of dangerous sexual behaviors.
- Avoid sharing all those objects – including razors, scissors, needles, and toothbrushes – that can penetrate the skin or mucous membranes.
- If you have decided to perform a tattoo, make sure that the procedures for disinfection and sterilization of the instruments are put in place correctly.
- Diagnosis
Several tests can be used to diagnose a sexually transmitted infection:
- Specialist physical examination.
- Blood tests
- Urine analysis
- Examination of biological fluid samples
- Treatments
The treatment choice depends on the type of infection the patient suffers from. Most STIs caused by bacteria are easier to treat, while STIs caused by viruses can be tracked over time, but they can't be cured permanently.
Antibiotics administered for local or systemic use are used in the case of sexually transmitted infections caused by bacteria and protozoa. It is best to avoid sexual activity until treatment is done and any injuries have healed.
In the case of viral infections, antiviral therapies are used (as in the case of herpes) or local surgical treatments (as in the case of HPV).
In the case of HIV, although therapies have not yet been developed that can permanently eliminate the virus, current treatments can keep it under control for many years, and mortality caused by this disease has decreased in recent decades.
Gonorrhea
Gonorrhoea is one of the most common sexually transmitted diseases in the world. It is provoked by a bacterium, Neisseria gonorrhoeae, capable of infecting the urethral pathways in men and the urogenital pathways in women.
This bacterium needs a warm and humid environment to grow and reproduce, and the female genital organs and the urethra (both in women and men) are the ideal environments. However, the infection can also develop in the mouth, throat, eyes, and rectum.
Since gonorrhoea sometimes presents few symptoms, making the diagnosis complicated makes it easier to get infected. If left untreated, it can have serious consequences: in women, it can damage the tubes, causing infertility and increasing the risk of ectopic pregnancy. In humans, it can cause epididymitis, an inflammation that, if left untreated, can lead to infertility.
Contagion occurs through unprotected sexual intercourse – vaginal or oral – with an infected partner. The infection can also be transmitted from mother to child during childbirth.
Gonorrhoea, especially in women, is often asymptomatic. When symptoms occur, they are usually mild and difficult to distinguish from other infections affecting the vagina or bladder. Although the symptoms frequently appear benign, complications can also be severe and lead to infertility. When present, the symptomatology in women includes:
- Burning during urination.
- It increased vaginal secretions.
- Blood loss between menstrual cycles
In men, symptoms can appear over a somewhat variable period – two to thirty days after infection. They include mainly:
- Burning during urination.
- Loss of colour tending to white, yellow, or green from the urethra.
- You may also experience pain or swelling in your testicles.
Rectal infections are usually asymptomatic but can occur, both in men and women, with:
- Leaks
- Anal itching
- Bleeding
- My bowel movements are excruciatingly painful.
You must avoid gonorrhoea infection:
- To avoid casual sexual encounters
- Avoid sexual intercourse with infected partners
- Sex protection
- Use the condom correctly
The diagnosis is generally easier to make in men than in women. Since gonorrhoea is often asymptomatic, laboratory tests must be used to make the diagnosis. The samples to be analysed are taken with swabs from the most frequently infected body parts (cervix, urethra, rectum, and pharynx).
The bacterium can be examined under a microscope directly or grown in the laboratory for culture examination.
Since gonorrhoea is a bacterial infection, the treatment is based on antibiotics. Antibiotics that are started in the urine are used for maximum results.
In recent years, Gonococcus has become resistant to many antibiotics, so the antibiogram is often used to determine which antibiotic will work best.
Chlamydia
Chlamydia is a sexually transmitted disease caused by infection of a microorganism, Chlamydia trachomatis. This bacterium is mainly transmitted through sexual intercourse. Vertical transmission from mother to child during pregnancy is also allowed. Chlamydia infection predominantly affects women but does not disdain the male sex. The disease is almost always asymptomatic. It can cause subtle symptoms ranging from vaginal irritation to burning and irritation during urination to feeling weight and pain in the pelvic and vaginal blood discharge.
If the infection progresses, the tubes and ovaries may be affected, forming inflammatory processes at their expense (hydrosalpinges, tubal abscesses, adhesion syndromes) and aggravating symptoms (abdominal pain, fever, diarrhoea, nausea). Inflammatory processes affecting the pelvis and tubes decrease the function of the reproductive organs, with a risk of infertility.
Frequently, therefore, its very nature as a "silent" disease leads to neglect of the risks, which, on the other hand, in some cases, can be very important. Suffice it to say that Chlamydia is one of the most widespread sexually transmitted diseases globally, along with Gonorrhea and Syphilis (in the past called venereal diseases). For this reason, when there are even transient but abnormal symptoms, they should be reported immediately to the attending physician for the appropriate examination.
Chlamydia is a bacterial infection caused by a microorganism, Chlamydia trachomatis. Among sexually transmitted infections, it is among the most widespread. It is more frequent in women but affects men and women indifferently, with a peak around the age of twenty, that is, at the beginning of active sexual life. The bacterium is spread mainly through unprotected sexual contact, both vaginal and oral, and from mother to child during pregnancy.
The disease is caused by Chlamydia trachomatis, spread through sexual contact and from mother to child.
The symptoms of chlamydia are often mild and transient. They generally include:
- Urinary discomfort (urination pain)
- Reddened spots on the genitals
- Pain in the lower abdomen or a sense of weight
- Genital and pubic itching
- Vaginal discharge in women
- Painful sexual intercourse in women (dyspareunia)
- Testicular pain in men
- Rectal pain in men and women:
- Enlargement of the inguinal lymph nodes
Prevention of sexually transmitted diseases is achieved by practising a correct sexual life (hygiene during and after intercourse, use of condoms, and attention to the choice of sexual partners). In sexually transmitted diseases, the condom is not always enough to completely protect against diseases, but it is the most effective means of reducing the risk of infection.
Diagnosis of pathology is sometimes quick and straightforward. Generally, it is performed by:
- • A vaginal and cervical swab, in the case of women, urethral or in the case of both sexes
- • A cultured urine test for men and women to detect the presence of the bacterium
Sometimes the diagnosis is more complex and is carried out only through laparoscopy. This endoscopic examination is carried out by introducing an optical instrument connected to a camera into the abdomen. Laparoscopy makes it possible to find adhesions in the pelvic organs and changes in the tubes and ovaries caused by acute or long-term inflammation.
Chlamydia is treated with targeted antibiotics. On average, two weeks of treatment are required, during which the antibiotic prescribed by the specialist is taken. The antibiotic can eliminate the infection but can't fix the damage the microorganism did to the organs.
HPV infection (Papillomavirus)
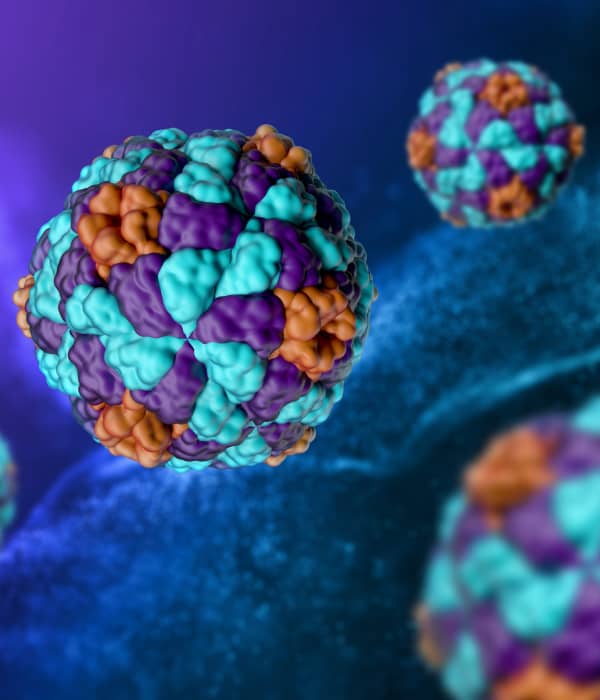
HPV (Human Papilloma Virus) constitutes a family of over one hundred different viruses. Most HPVs cause benign lesions such as warts that affect the skin (of the hands, feet, or face) and papillomas that affect the genital and oral mucous membranes. Most genital HPV infections regress spontaneously. However, a small wart can slowly progress towards a tumour form. Cervical cancer is, in fact, almost always related to the presence of HPV.
What is HPV infection (Papillomavirus)?
Infection with humans The effects of papillomavirus vary greatly depending on the type and family to which the viral strain you are exposed belongs. Generally, the virus replicates by exploiting the cells of the skin and mucous membranes and promoting excessive growth (hyperplasia) that causes the typical formations: warts and papillomas of the skin and mucous membranes. These growths are frequently coated with a layer of keratin (hyperkeratosis), characteristic of some forms of infection.
The most dangerous types of HPV are, however, those that cause malignantly evolving lesions in the upper respiratory tract – larynx, pharynx, tongue, tonsils, palate, nose – or in the male and female genitalia – glans, penis, scrotum for men; perineum, vagina, uterus, cervix for women.

Genital infection with the human papillomavirus is transmitted through sexual intercourse; it is, in fact, one of the most frequently transmitted sexually transmitted diseases. It is permissible that transmission can also occur with physical contact if there are active viral cells and if lacerations, cuts, or abrasions are present in the skin and mucous membranes. Generally, the most dangerous respiratory tract infections or oral cavity infections are transmitted through oral sex—through contact, therefore, between the mucous membrane and the genitals.
People with a particularly vulnerable immune system are more exposed to the risk of contagion. With much lower frequency, the infection can be caused in places where promiscuity is created (such as public showers, swimming pools, and barracks) by contact with surfaces previously used by carriers of the infection.
The symptoms of the human papillomavirus vary according to the type of infection. Most of the time, common warts, plantar warts, and genital warts are the most common signs of illness.
Genital warts (called warts) can be located on the external genitalia, inside the vagina, around or inside the anus, and on the perineum (the skin region between the vulva and the anus). These lesions manifest as small growths, sometimes arranged in clusters, with a shape reminiscent of a cauliflower. In other cases, the lesions are flat and tend to overlap.
Most lesions caused by HPV are asymptomatic, but warts can cause discomfort, itching, or discomfort in some cases. The strains of HPV that cause cancer in the genital areas, on the other hand, don't cause warts. Instead, they cause changes in the genital mucous membranes (usually in the uterine neck) that don't cause any symptoms.
To avoid HPV infection, it is essential to remember a few simple rules. If you frequent common areas, such as changing rooms or swimming pools, keep your feet clean and dry and wear shoes or slippers.
To avoid the spread of warts from the hands to the mouth, it is necessary not to bite your nails.
The transmission of genital warts can be reduced by decreasing the relationships at risk, whether promiscuous or occasional and always using the condom (which allows for neutralising, if not all, the most frequent modes of contagion). It is also essential to take care of personal hygiene.
Sexually active women must periodically undergo a gynaecological examination and a Pap test, which is better if combined with the search for viral DNA.
For some years, a vaccine has been on the market that protects the cervix from the most dangerous strains of HPV. Scientific studies have promoted its administration to the adolescent population of both sexes to reduce the risk of contagion. Recent studies would also seem to support the vaccine's use for the adult population or those already infected with the virus.
The doctor can make a clinical diagnosis of HPV infection by looking for the typical lesions.
The diagnosis of cytological and histological alterations (i.e., cells or tissues) caused by potentially oncogenic HPV strains is instead obtained through the execution of the Pap Test or special tests for the detection of viral DNA. If necessary, targeted biopsies are carried out on the genital mucous membranes under the control of a particular instrument (the colposcope) that allows for the enlarged visualisation of the examined tissues.
It is possible that lesions caused by HPV heal spontaneously without any treatment. However, it is good to know that the virus can still be present in the human body even when warts disappear.
Skin warts can be treated with topical solutions based on salicylic acid or trichloroacetic acid, or with creams with antiviral action, or be removed with local surgical treatments (diathermocoagulation, laser therapy, cryotherapy).
Genital warts are usually vaporised through diathermocoagulation or laser treatments.
Partially removing the precancerous lesions from the uterine cervix lets the woman keep her ability to have children.
Genital Herpes

Genital herpes is caused by the Herpes simplex virus, a virus of the same family as the one that affects the lips. However, when this virus affects the genitals, both male and female, it can manifest itself with more significant discomfort and even greater complications than the lesions it causes on the lips. Sometimes, however, it does not cause any symptoms, so the person does not know he is contagious.
It is generally transmitted sexually and can affect the scrotum, the tip of the penis in men; in women, the vulva, vagina, and cervix; the urethra and the perianal area. It manifests as pain, burning and itching, some with fever, migraine, muscle pain, and difficulty urinating. It presents with small, grouped lesions that tend to regress on their own within a week or two.
What is genital herpes?
Genital herpes is a widespread viral infection that is transmitted through sexual intercourse. It is manifested by whitish vesicles grouped in an inflamed area that provoke itching, pain, and discomfort.
Genital herpes is a sexually transmitted virus. It seems that the virus is more easily sent from man to woman. Therefore, it is transmitted during intercourse through skin contact if the partner is sick. Often, the virus does not cause symptoms; consequently, the person may be unaware of it. The causes of infection can also be attributed to the immune system's weakness in cases of stress, illness, and during menstruation.
The first symptoms of genital herpes are pain and itching.
A few days after infection, small red or white blisters may form. Often, superficial or deeper painful ulcerations are formed, which can bleed. They usually heal within a few weeks on their own. The infection tends to come back in the next stage and causes flu-like symptoms.
- fever
- muscle pain
- headache
- general malaise
- swollen inguinal lymph nodes
Prevention of genital herpes is analogous to all other sexually transmitted diseases and therefore requires sexual abstention when you know you are affected by the virus or using a new condom during each sexual act.
Women who are pregnant or suspect they are pregnant should notify their doctor, who will assess the need for antiviral therapy.
The diagnosis of genital herpes is obtained with a simple visit to the specialist. The observation of the sick part is enough to reach the diagnosis.
The cytological examination can be done by taking cells from the vesicles to get a complete picture.
Other diagnostic means are often excessive, given the spontaneous remission of the virus in a few weeks. However, it is possible to detect the previous or current presence of the virus through a blood test for specific antibodies.
Systemic therapy with antiviral type Acyclovir allows for reduced symptoms but does not prevent a recurrence. The treatment is carried out both locally and systemically. Locally, you can apply antiherpetic creams, but they are not helpful in the vagina or cervix.
HIV AIDS Virus
AIDS (acquired immunodeficiency syndrome) is an infectious disease caused by HIV (human immunodeficiency virus). The main action of the virus is to reduce the body's immune defences. The virus destroys CD4 cells that perform a necessary defensive action against other infections.
There are no cures or vaccines for the eradication of the infection. Antiretroviral treatment, which is used to treat HIV infection now, is a combination of drugs that stop the virus from multiplying and slow down the destruction of the immune system and, therefore, the spread of the disease.
The execution of the HIV test, which is carried out by law anonymously and quickly, is the only tool available for early diagnosis.
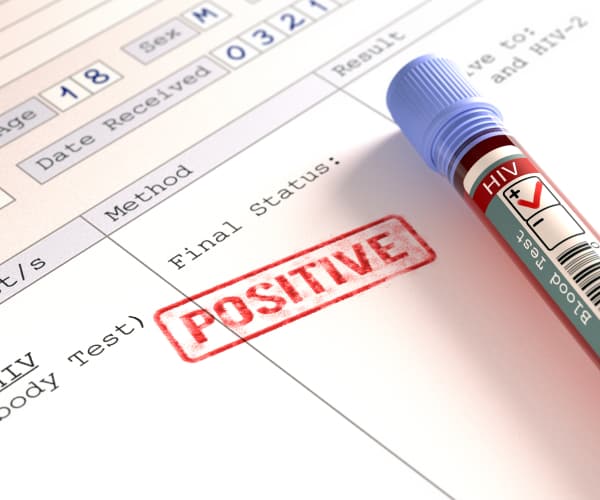
HIV is transmitted at any stage of the disease through unprotected sexual intercourse, contact with blood, vertical transmission between mother and baby during pregnancy, childbirth, and breastfeeding.
HIV has a high capacity for replication, especially in the early stages of infection. It uses white blood cells to replicate itself, destroying them and leaving the body devoid of these cells. It can take many years for AIDS, which is caused by a weak immune system, to go from an infection to a "full-blown" disease.
HIV is transmitted at any stage of the disease through unprotected sexual intercourse, contact with blood, vertical transmission between mother and baby during pregnancy, childbirth, and breastfeeding.
Two distinct stages generally characterise the manifestation of the virus. In the first stage, a few weeks after infection, patients can complain of symptoms of a flu-like syndrome characterised by fever, swelling of the lymph glands, joint and muscle pain, skin manifestations, and night sweats. Infection progression differs from person to person. In some cases, it may remain symptom-free (clinical latency) for many years.
If the infection isn't treated early with antiretroviral therapy, it can lead to AIDS. At this point, "opportunistic" pathogens already in the body can cause infections, leading to diseases that could get worse and kill the person.
The only way to prevent infection is to avoid behaviours that can expose you to the risk of contagion. In cases of sexual intercourse, the use of a condom is necessary.
The diagnosis of HIV infection can be made following a blood test (ELISA test) that can detect the presence of antibodies specific to the virus. A positive ELISA test must always be confirmed by a further test (Western Blot test).
The virus may still be undetectable to the test; this is the so-called "window period". You are already infected and contagious, but seroconversion has not yet occurred.
There are now early tests to determine whether you are HIV positive (p24 antigen test, combined tests). The test is simple; it consists of a blood sample conducted anonymously by law.
There is currently no cure for the eradication of HIV infection.
Treatment of HIV infection consists of controlling the virus through a combination of drugs that block the replication of the virus, reducing viral load and, consequently, destroying the immune system.
Hepatitis A
Hepatitis A is a contagious liver infection caused by the hepatitis A virus, also known as the HAV virus, one of the viruses that cause inflammation and can impair the functions of the liver. The disease is spread by eating or drinking something with the virus or by coming into contact with someone who has it.
What is hepatitis A?
The average incubation period of the disease is about four weeks; after healing, the patient is wholly immunised against the virus. It is a very resistant pathogen, which can withstand high temperatures and very acidic environments. Still, it is a disease that never becomes chronic and is considered dangerous only when it occurs in older people or those with other health problems.
Often, in very young children, it is almost asymptomatic. In milder cases, there is no need to treat hepatitis A, and most people who get it get better without their livers being permanently damaged.
Once the disease has been defeated, all people infected with the HAV virus are permanently immunised by the virus.
The hepatitis A virus spreads mainly through faecal matter. Contact with even minimal amounts of contaminated faeces quickly leads to contagion. The virus spreads to the liver, causing inflammation and infecting the infected person's faeces. In Italy, the improvement of general hygienic conditions has led to a decrease in the risk of contagion. Still, if you stay in other places where hepatitis A is common, it is best to get vaccinated as a precaution.
Some of the modes of contagion can be:
- Handling food by infected people who have not washed their hands carefully after going to the bathroom.
- Contamination of drinking water using even minimal amounts of viruses.
- Ingestion of seafood or fish contaminated by sewer discharge.
- Sexual contact, or in any case, situations of promiscuity with infected people (even asymptomatic).
The symptoms of hepatitis A typically occur a few weeks after infection, once the incubation period has elapsed, during which the pathology is equally contagious. Among the most obvious symptoms are:
- Fatigue
- Nausea, vomiting, and loss of appetite
- Abdominal pain and discomfort, especially in the liver area.
- Yellowing of the eyes and skin (jaundice)
- Dark coloured urine
- Light fever and muscle pain
The symptomatic phase usually lasts 8–10 weeks, although it can sometimes continue for up to six months. Hepatitis A, on the other hand, may not cause any symptoms in some people, especially children.
The diagnosis of hepatitis A is made through simple blood or stool tests or, in the symptomatic phase, through a medical examination.
There are no specific treatments for hepatitis A. Most of the time, the problem goes away on its own after a couple of months, leaving no permanent damage to the liver. Because of this, treatment is often based on how the person feels.
- Trying to rest and avoid strenuous physical activities is a good idea because the main symptom is noticeable ease of fatigue.
- Nausea and loss of appetite can become problems for those affected because not eating can accentuate fatigue. One strategy could be to make more meals than usual, albeit with smaller amounts of food.
- Try not to overstress the liver with medication and alcohol to get a faster course and milder symptoms.
The hepatitis A vaccine can prevent infection and is commonly given in two doses, about six months apart. The vaccine is recommended for all people at risk due to their daily activities or for whom infection could constitute a severe risk. It's a good idea to discuss the opportunity to get vaccinated with your doctor.
When travelling abroad, it is good practice, in general, to consult the indications of the Ministry of Health regarding potential risks related to the areas to be visited and preventive vaccinations that can reduce the risk of contagion for some diseases.
Getting sick is much less likely if you always wash your hands before and after going to the bathroom and before and after touching food and drink
Hepatitis B
Hepatitis B is a pathology that affects the liver and can have severe effects. This disease can become chronic in some individuals, leading to liver failure, cirrhosis, and liver cancer. There is antiviral therapy for but no cure for hepatitis B, and the vaccine prevents infection.
What is hepatitis B?
Hepatitis B, caused by the HBV virus, is a disease that is transmitted quite easily: the virus can be carried by blood, semen, and vaginal fluids. Contagion cannot occur through random contact such as handshakes, hugs, kisses, sneezing or sharing cutlery and glasses. It is estimated that about a quarter of the world's population has been infected with the HBV virus at some point in their lives. Even with severe symptoms, most adult people infected with the virus fully recover without lasting liver damage.

The hepatitis B virus, which is transmitted through sexual contact, parental or by exchange of infected blood, when it settles in the liver, begins to multiply, replicating in the liver cells (hepatocytes) and leading to inflammation and the appearance of symptoms (acute phase); or it remains latent, even for a long time, slowly damaging the liver of the infected person. Hepatitis B can manifest itself both in chronic and acute forms.
- Chronic form
If the infection lasts more than six months, it is called chronic hepatitis. This happens because the immune system cannot eliminate the virus; in that case, the pathology can last for years and lead to severe problems such as liver cancer, cirrhosis, and chronic liver failure. Hepatitis B becomes chronic in most children who inherit hepatitis B from their parents or contract it before the fifth year of life. Chronic hepatitis B can evolve at any time into an acute form
- Acute form
The acute form of hepatitis B lasts less than six months, especially in those who contract the virus in adulthood, because the immune system, if healthy, usually manages to develop specific antibodies and defeat the pathology within a short time.
The symptoms of hepatitis B typically occur about three months after infection, after the incubation period, during which the pathology is equally contagious. Among the most obvious symptoms are:
- Fatigue
- Nausea, vomiting, and loss of appetite
- Abdominal pain and discomfort, especially in the liver area,
- Yellowing of the eyes and skin (jaundice)
- Dark coloured urine
- Joint pain
It is not unusual for children and sometimes even adults to have the disease with almost no symptoms. Symptoms only show up when the liver damage is already severe.
Sometimes, doctors recommend hepatitis B tests in people with no symptoms because, as mentioned, the symptoms of hepatitis B may sometimes not manifest until the disease has seriously compromised the liver.
The correct diagnosis of hepatitis B can be made by studying the dosage of specific viral markers. Tests for hepatitis B virus infection include serum or blood tests that detect viral antigens or antibodies produced by the host subject. These molecules are contained in the blood of those who have contracted the disease. The interpretation of these tests is, however, quite complex.
Individuals at risk of hepatitis B should periodically check their condition through specific tests. Anyone who thinks they fall into these categories should discuss this with their doctor.
- If you take intravenous drugs,
- Anyone living with a person who has contracted hepatitis B
- Who is HIV positive?
- Anyone who has had sex with infected individuals
- Who has received hepatic dialysis treatments?
- Who comes from countries where hepatitis B is endemic or has lived in those countries?
- Who takes or has taken immunosuppressive medications?
- Pregnant women
- Men who have had sex with other men
Those who present the infection in acute form often do not need any treatment. In this case, it is best to focus on alleviating symptoms. On the other hand, patients in whom hepatitis B becomes chronic are usually treated with antivirals selected by the hepatologist based on the characteristics of the individual patient (age, general health condition, possible presence of concomitant pathologies). Depending on the opportunity, a liver transplant can be evaluated in cases of impaired liver function.
In Italy, vaccination against hepatitis B is recommended in newborns and, in general, in children under 12 years of age.
The vaccine is recommended for all people at risk due to their daily activities or for whom infection could constitute a severe risk. It's a good idea to discuss the opportunity to get vaccinated with your doctor.
When travelling abroad, it is good practice, in general, to consult the indications of the Ministry of Health regarding potential risks related to the areas to be visited and preventive vaccinations that can reduce the risk of contagion for some diseases.
Hepatitis B and other sexually transmitted diseases can be avoided if you pay attention to your sexual partners and use a condom, even if you only do it once in a while.
Attention to where and how you do piercings and tattoos (using sterile instruments and excellent general hygienic conditions) can also help protect yourself from these diseases.
Hepatitis C

Hepatitis C is a pathology caused by the HCV virus that attacks the liver and leads to inflammation. Most people with hepatitis C do not experience symptoms; many don't realise they're suffering from hepatitis C until liver damage emerges, years or even decades later than the infection.
What is hepatitis C?
The HCV virus is one of the many viral agents that can infect the liver, but HCV infection is considered the most serious one affecting the liver. The virus is transmitted through contact with infected blood, typically through exchanging infected syringes or, less efficiently, by sexual or parenteral transmission (from mother to child). The most significant risk associated with this pathology is chronicization, which occurs in patients who are not treated (often because there is no symptom). This pathology can result in severe consequences such as liver failure, cirrhosis, and liver cancer; chronic hepatitis C is thought to cause one in every four liver cancers.
Hepatitis C, as mentioned, is transmitted through direct contact with blood infected with the HCV virus. The most common transmission modes are:
- Exchange of infected syringes: People who use intravenous drugs are more likely to get sick if they use the same syringe as a person who is ill.
- Blood transfusions or organ transplants that took place before 1992: It is possible that, given the poor reliability of blood tests before this date, the virus was transmitted through transfusions or organ transplants. Improved screening tests make it highly unlikely that this could have occurred after 1992.
- Although the chances are not high, the virus may spread from an infected mother to a child during pregnancy.
- Sexual contact: In rare cases, the HCV virus can be transmitted through unprotected sex.
- Tattoos or piercings: Despite the recent improvement in the hygienic conditions of studies that practise tattoos and piercings, there is a possibility that, when hygiene rules are not correctly applied, the HCV virus will be transmitted through these practices.
The disease usually does not produce any symptoms during its early stages. The first symptoms are very mild and easily confused with those of other pathologies, so it is estimated that most infected people never become aware of the infection. In any case, among the most common symptoms are:
- Fever
- Nausea and reduced appetite
- Fatigue
- Sensitivity in the liver area
- Muscle and joint pain.
Tests for the diagnosis of hepatitis C help the doctor direct the affected patient toward a lifestyle and a series of practical measures to prevent the liver from suffering the most significant damage. Since this pathology often causes severe damage before entering its symptomatic phase, periodically undergoing tests is a good idea, especially for those who fall into the categories at risk of infection. All people who:
- Have used intravenous drugs.
- Have had sex with people at risk.
- Have undergone transplants or transfusions before 1992.
- I have undergone hemodialysis for long periods.
- You were born to a mother infected with hepatitis C.
- They have detected significant abnormalities in their liver function tests.
- Have worked as doctors, nurses, or volunteers in environments or with people at risk of contagion.
Blood testing for HCV infection can be helpful for various reasons; in addition to enabling the certainty of the diagnosis, it is also possible to evaluate the amount of virus present in the blood (viral load) and the genotype of the virus. These two parameters can help the doctor determine what may be the best therapeutic options.
Finally, if your doctor suspects severe damage to liver function, he may prescribe a liver biopsy to ascertain more accurately. Liver biopsy is an invasive procedure, although it is generally safe and may require, in some cases, hospitalisation of the patient.
Treatment of hepatitis C is not always necessary. Monitoring liver values once in a while is enough for people with mild liver damage and no obvious disease symptoms.
Most patients who need treatment take antiviral drugs that allow the complete elimination of the virus. Typically, complex therapies are prescribed, lasting many months, the composition and duration of which vary depending on the genotype of the virus. These treatments can have significant side effects.
Liver transplantation may be considered if the patient's overall health is good, but the liver is compromised by hepatitis. In any case, transplantation doesn't always get rid of the disease, so antiviral treatments must still be done even after transplantation.
Finally, doctors often recommend specific vaccines for hepatitis C sufferers since the possible infection with the viruses of these pathologies could create more severe complications and more incredible difficulty in treating hepatitis C.
Although several trials are underway, an effective vaccine against the HCV virus, which causes hepatitis C, is not yet available on the market. Prevention, therefore, consists of eliminating, as far as possible, risk factors. In this sense, the spread of disposable syringes has already significantly reduced the risk of contagion among drug addicts. Sexual intercourse, mainly when occasional, protects against many sexually transmitted diseases. Finally, those who decide to get a piercing or a tattoo should carefully check the hygienic conditions and comply with the rules of those who work in the studio they have settled on relying on.